Breast reduction is known medically as reduction mammoplasty or reduction mammaplasty. There are many described methods, which have been reduced to a common denominator in the following:
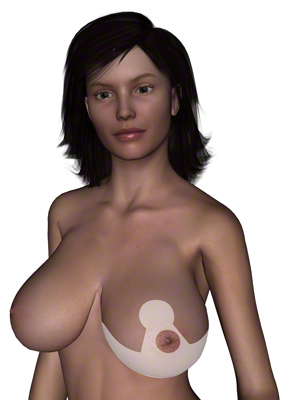
- Inverted T-breast reduction
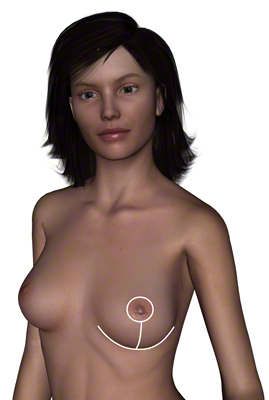
- Vertical incision breast reduction
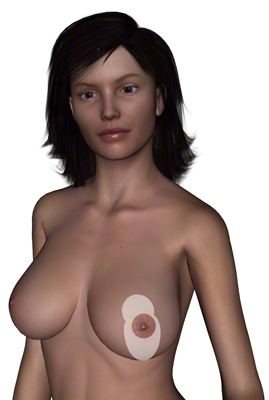
- Reduction mammoplasty with periareolar incision (reduction is only possible to a limited degree)
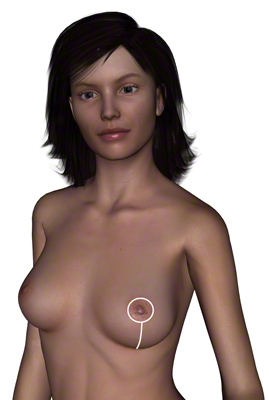
- Reduction mammoplasty with internal muscle bra fixation

Content
Yuveo Klinik
Characteristics of breast reduction
Breast reduction can be performed in different ways depending on the incision type.
Inverted T-incision
Vertical incision
l-incision
Internal suspension
T-incision and vertical incision during breast reduction surgery
The inverted T-incision is also called the anchor incision.
The breast reduction with the inverted T-incision is certainly the most utilized incision technique. The scar that results runs around the areola, then vertically down to the inframammary fold and there transversely in the fold, thus like a “T” standing on its head. Using this technique of breast reduction, a remarkably large amount of skin can be removed in the horizontal and vertical directions. Thereby, a good end result without irregular areas or folds can be expected, even with large and/or slack breasts.
The end result is visible relatively quickly, not as with the breast reduction using the vertical incision, in which the scar and skin contraction take a long time to set. However, the technique is associated with a long scar line. Therefore, if possible, this technique should not be utilized in women who tend to develop severe bulging scar buildup (hypertrophied scars or keloids).
The vertical incision is a minimal-scar technique.
The breast reduction with the vertical incision belongs to one of the minimal scar techniques. The scar goes around the areola and then vertically down to the inframammary fold. The incision is not carried transversely in the inframammary fold. Thereby the space from the nipple to the inframammary fold and the excess skin located there is too great. Therefore the skin in this area is detached from the fat tissue, so that it can contract better. In addition the vertical suture is applied as a purse-string suture, to diminish the space between the nipple and the inframammary fold. Because of this, small skin wrinkles are produced which should regress with time as the skin contracts.
One relies on the tendency of the skin to contract, and this is certainly very good at a young age. This also functions amazingly well with a smaller breast reduction or a breast lift. If the skin quality is no longer optimal, however, the skin contraction will not occur to the desired degree. That also applies to a larger breast reduction. In such cases, the wrinkles in the area of the vertical scar remain visible. The space between the nipple and inframammary fold becomes greater again, and the breast sags. Surgical revisions may then be planned, and, upon acceptance, can lead to beautiful results with a scar in the inframammary fold. One usually waits 6 months after the breast reduction before deciding if such a follow-up operation is necessary. After that, the findings will not change appreciatively.
The probability of requiring surgical revision can be decreased. If the horizontal excess skin is greater than expected, one can minimize this through widening the incision in the inframammary fold. The result is the “small inverted T incision.”
FAQ: Breast reduction
What are the indications for breast reduction?
Breast reduction (reduction mammoplasty) is associated with the medical term macromastia, which describes breasts that are too large. Macromastia is considered to be one of the breast deformities.
Many women suffer with breasts that are too large. They often have the feeling that other people gawk at them because of their exorbitant size. This often leads to a subconscious bent-over position of the thoracic spine in an attempt to conceal the breasts. In addition, patients desiring a breast reduction usually report a list of symptoms that result from the excess weight of the breasts. For example, the patients frequently complain of back and neck pain. In this regard, 80% of the women feel relief immediately after the breast reduction. Because of the weight, tightness of the shoulders develops from the bra. Maceration (intertrigo) and fungal infections develop in the fold under the breasts, especially in summer. Poor posture caused by the weight can lead to signs of wear in the thoracic and cervical spines. Sports activities are hardly possible. It’s a challenge to find clothes that fit well.
Conservative therapy for large breasts is useless, because the real problem, the heavy weight of the breasts, cannot be corrected through physical measures and psychotherapy. This can only be achieved through breast reduction. In the case of preexisting cervical spine and thoracic spine syndromes, the breast reduction can lessen the weight and thereby alleviate the discomfort and delay further deterioration
In the case of being overweight in general, an attempt should be made to reduce weight before a surgical breast reduction is performed, because, for many women, more than the average amount of weight that is lost comes from the breasts. Sometimes breast reduction becomes unnecessary after weight reduction. However, in many cases, because of resultant excess skin, a breast lift is desired.
When breasts are abnormally large in men, the condition is called gynecomastia. Here the breast reduction is carried out by means of liposuction and / or through a small incision. Only in extreme cases does a breast reduction need to be performed as with women.
What happens during a breast reduction?
During the reduction mammoplasty, glandular breast tissue as well as fat tissue and skin are removed. The areola is incised and thus reduced in size. Furthermore, the areola must be repositioned upward. For this, there are numerous described techniques and incisions. It is not possible to operate without scars! One can only try to leave the least scarring and the least conspicuous scars possible. However, the minimal scar techniques have their limit.
What kinds of incisions are available for breast reduction surgery?
The techniques described in the literature for breast reduction are diverse. For the most part, they distinguish themselves from each other only insignificantly. The most significant basic techniques can be well described as the inverted T-incision, the vertical incision and the L- incision, and they are used in a fashion similar to those used with the breast lift.
What is the L-incision?
The L-incision is quite similar to the vertical incision. To decrease the above-described excess skin in the horizontal direction somewhat, the incision is extended outward in an “L” form. More often, however, the “small inverted T incision” is used, because the excess skin in the center can be better corrected.
What is meant by breast reduction with internal suspension?
To give the breast more stability and to provide a longer lift effect for the breast reduction, there are several techniques by which one constructs one or more lobules from the deep skin layer (corium) and / or from the fat tissue and the breast’s own glandular tissue. These lobules are attached to the pectoral muscle sheath or to a firm fibrous layer in the fat tissue (Scarpa’s fascia). Thereby it is also possible to shape the breast. The fat lobules or glandular lobules then act as an autologous (from one’s own body) implant and give the breast a better form. The goal of this form of breast reduction with suspension is to take the main load off the skin and skin sutures to enable a low stress wound closure and to prevent or delay renewed sagging.
What about the nipple-areolar complex = nipple + areola?
The nipple-areolar complexes are somewhat maltreated during breast reduction and breast lift surgeries. That is to say, they are reduced in size and repositioned upward. When the upward relocation is not too far, this can be accomplished by means of a cutaneous pedicle, which assures the blood supply for the areola. If this is too long, or gets kinked or is squeezed too strongly, the blood supply can be gravely impaired. The areola becomes pale or blue (insufficient blood supply). If the perfusion cannot be improved, then it is possible that, in most cases, only a portion of the nipple-areolar complex could die off. That would mean a protracted healing process, which would depend on the extent of the dead tissue. Today, however, this is to be expected extremely rarely, even with a larger breast reduction.
In extreme cases, if the nipple must be raised over 10 cm, the possibility of transplantation of the nipple-areolar complex should be mentioned in the counseling interview. That means that the areola is completely detached and then sutured into its new bed. Immobilization with pressure for the first 5-7 days is vital for such a full-thickness skin graft, to allow it to grow in. One can see if it is successful after about 1-2 weeks.
These days, it is only necessary to perform nipple-areolar complex grafting in exceptional cases of breast reduction surgery.
When is liposuction used in breast reduction surgery?
For women with the goal of breast reduction, Liposuction has no significance. The reason for this is obvious. It’s true that the weight of the breast can be reduced by liposuction, but not the skin covering. The result would be a severe sagging of the breast.
Nevertheless, used in conjunction with breast reduction, liposuction can be of good service. Large breasts often have a wide base, meaning that they have an extension that reaches to the underarm. These extensions could only be corrected in the primary operation with a very long incision in the inframammary fold. Here liposuction comes into play, and with its help one can extract the tissue extensions either in the primary operation or secondarily (after 6-12 months), in order to reduce the volume without lengthening the incision.
Should a mammogram be arranged before a breast reduction?
Before a planned reduction mammoplasty, women who are older than 35 – 40 undergo a mammogram to be able to respond to suspicious findings appropriately. A mammogram is also recommended 12 months after the breast reduction, so the radiologist has new baseline findings and can compare and classify later changes. After this operation there is neither an increase nor a decrease in the occurrence of breast cancer. Cancer screening is of course necessary after the breast reduction.
Can sagging occur after breast reduction?
After the breast reduction, the breast is, of course, exposed to the aging process and will become saggier with time. Because the weight, which had put stress on the skin, was reduced, the breast sagging clearly occurs later and more slowly than would have been the case without the breast reduction.
What about postoperative care?
- Drains
At the end of the operation, two suction drains (= Redon Drains) are inserted, which can be withdrawn after 1-5 days. - Compression
It is important to keep quiet in the first 24 hours after the breast reduction, so that small vessels that had been tied off do not open up again. By wearing a compression bandage for one night, the risk of bleeding is additionally minimized. - Showering
Through use of a water-tight bandage, one can carefully shower shortly after the drains are removed. Before that, the bandages must remain dry. - Stitches
Resorbable stitches do not need to be removed. Non-resorbable stitches are removed after 10-14 days. - Bra
As a rule, use of a bra is recommended for 4-6 weeks. - Re-emergence of breast glandular tissue
The very rare re-emergence of breast glandular tissue after a breast reduction is described in the literature. It occurs predominately in young women, or is caused by hormones as a consequence of pregnancy. - Sports
In general, sports should be avoided for 6 weeks after a breast reduction. This pertains particularly to types of sports in which vigorous movement of the shoulder girdle and the chest is expected. Lighter sports may be practiced 1-2 weeks earlier. - Sleeping on the stomach
Sleeping on the stomach (prone) is only allowed after the 7th week.
What complications can occur during breast reduction surgery?
In the following, the most important complications that can occur with a breast reduction are briefly described:
- Postoperative swelling
After the breast reduction, a certain amount of postoperative swelling, which may be uneven side-to-side, is normal. It can be in the form of smaller bruises or more pronounced in wound effusions. A certain amount of induration (hardening) is also normal postoperatively. These changes improve in the first postoperative weeks. - Hematomas
In this surgery, large wound surfaces are produced. Therefore it is especially important to carry out meticulous hemostasis. With subsequent compression and insertion of drains, large hematomas in patients without clotting disorders are rare. The body can resolve smaller hematomas itself; larger ones require an operative removal on an as-needed basis. - Bleeding
This is avoided as a rule by use of careful hemostasis and compression. Items described under hematomas apply here as well. By removing the drains quite prematurely after the breast reduction, adherent vessels can open up and rebleed. - Disturbance of scar formation after breast reduction
So-called hypertrophic scars (or, in the worse cases, keloids) can occur occasionally in people with corresponding disorders. These can then be treated with special salves and, where appropriate, cortisone injections, among others, more or less successfully. If a disturbance of scar tissue is known, depending on severity, it must be seriously considered whether a breast reduction should be performed at all. - Infections
The risk of infection should be reduced through highly sterile conditions and, if necessary, antibiotic prophylaxis. If cysts are apparent during surgery, this becomes especially important. - Dog ears
Excess skin is present on both ends of the horizontal cut surfaces. The worse the findings, the more extensive the tissue that is removed during the breast reduction, and all the more extensive is the amount of excess skin that is ultimately removed. They are called dog ears because of the resemblance. Removing these surgically is only done with caution in breast reductions to prevent excessive widening of the scar. They can be reduced using special suture techniques. It is hoped that they will shrink within 3-6 months and eventually will not be visible. If the desired shrinking effect is not sufficient, then a small revision under local anesthesia can be carried out. - Skin sensation in the nipple after breast reduction
A worsening of sensation or numbness of the nipple after the breast reduction must be anticipated, the more so because the small afferent cutaneous nerves are, to a large extent, severed. However, for many patients, the sensation in the nipple is astonishingly good postoperatively. But there is also the possibility of complete numbness after the breast surgery. This is especially true when the nipple needs to be repositioned over 10 cm. - “Grief corner” (trouble spot)
Similar to that described in the breast lift and the tummy tuck, so-called “grief corners” can also occur with the breast reduction. This applies to the place in the inframammary fold at which the vertical and horizontal incisions meet in the inverted T incision breast reduction. Here the perfusion is diminished by the fact that three flaps of skin come together, and consequently, more tension is placed on the sutures. Delayed wound healing therefore occurs here more frequently. The scar can also be wider than in other parts of the suture line. A small scar revision can be planned for after about 6 months to be done under local anesthesia, when the scars are mature. - Tearing of the wound / sutures
With too much tension and too much movement of the chest, the sutures can become overstrained and tear. Therefore, especially in the first week after the breast reduction, one should take care of oneself. Movements of the arms, especially over the head, are to be avoided for several weeks. - Tissue necrosis
Especially in heavy smokers or with extreme breast masses, it is possible for the perfusion of the nipple to be insufficient. In that case, parts of, or even the entire nipple can necrose (die off). During the surgery, of course, the state of perfusion can be monitored. If the perfusion is insufficient, one can decide to do a grafting of the nipple and/or the areola. The graft is accepted in most instances. Of course, then the skin sensation is completely impaired, meaning that the nipple remains numb. It is important to avoid cigarettes before and after the breast reduction so that perfusion is not further impaired. - Wound serous effusion = seroma
In the breast reduction, relatively large wound surfaces exist, which can produce wound drainage, depending on individual predisposition. Usually this does not develop into changes that are worth mentioning. Sometimes smaller and mid-sized seromas develop, which resolve on their own with time. The larger seromas must sometimes be drained using a cannula. - Unsatisfactory cosmetic results
In the setting of an effective counseling interview, the expectations of the patient and the possible operative results should be brought into accord to prevent disappointments. For asymmetric, suboptimal scar healing, among other problems, surgical revision can provide a remedy. - Thrombosis and embolism after breast reduction
Thrombosis prophylaxis with Heparin and support hose is advisable. - The risks of narcotics / anesthesia will not be addressed here.
Checking the facts
Smoking must be stopped for 2 weeks before a breast reduction to minimize the risk of disturbance to wound healing.
The procedure must be carried out under general anesthesia and lasts about 2 hours.
The incision is dependent on the amount of tissue to be removed.
Depending on the extent of the breast reduction, a stay in the hospital for at least one night is allowed for.

